Home » News & Stories » Reducing the rate of hospital-acquired pressure injuries
Reducing the rate of hospital-acquired pressure injuries
Submitted by Katharin Bak, RN, MSN, Director of Nursing and Rachel Noyer, RN, WCC, Interim Inpatient Nurse Manager
Background
Valley Regional Hospital had three hospital-acquired pressure injuries in the first quarter of 2023 and subsequently completed a root cause analysis.
The RCA team included members from quality, risk/compliance, nursing leadership and staff RNs directly involved in patient care. The team identified gaps, including:
- staff failure to recognize/stage pressure-related wounds;
- lack of knowledge related to mandatory reporting of HAPIs;
- lack of a defined process for recognition/documentation/reporting;
- lack of education upon orientation and ongoing competency validation;
- inconsistent handoff processes between shifts;
- lack of individual responsibility and accountability around PI prevention; and
- lack of a hospital policy or any other supportive tool for nurses to reference.
Approach and collaboration
The team used the Institute for Healthcare Improvement’s Plan-Do-Study-Act cycle tool to guide a performance improvement project to address these gaps.
For the “Plan” phase, the team asked, “How can we reduce HAPIs on the inpatient unit?” They predicted that increased awareness, education and knowledge of the contributing factors related to PI development would reduce rates. The team collected PI data before implementing interventions.
The team involved nursing staff from the inpatient unit, emergency department and nursing leadership to assess current knowledge using the National Database of Nursing Quality Indicators Module 1, direct observations and discussions.
Based on results from the assessment, during the “Do” phase, VRH:
- completed the nursing quality checklist;
- incorporated a monthly chart review of skin assessments;
- created a PI identification and wound care process map to outline the necessary steps for staff to take;
- assessed staff knowledge;
- provided education/mandatory skills day, hospital policies and wound care resources;
- tracked PI with a quality dashboard; and
- implemented wound care nursing consults.
Results and impact
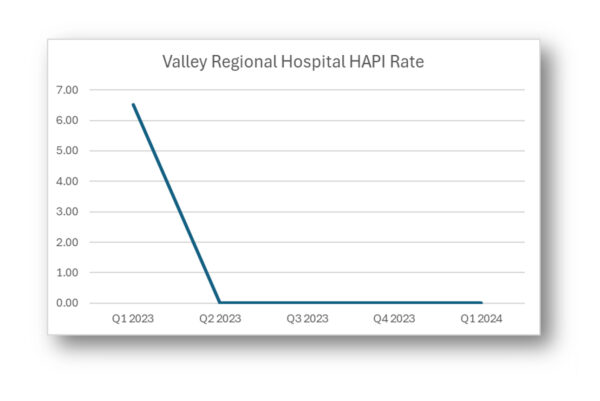
For the “Study” phase, the team analyzed the impact of these interventions on their predictions and found that increased awareness, education and knowledge of the contributing factors related to PI development did reduce HAPI rates.
The hospital increased its attention and focus on PI prevention and treatment and provided tools to support staff’s roles in preventing, assessing and treating PI and other wounds.
As a result, staff demonstrated more knowledge of PI staging, communication and documentation.
For the “Act” phase, the team implemented a prevalence study tool, included hospital-acquired injuries and infections in clinical staff orientation and continues to monitor staff competencies. VRH is also planning for the next PDSA initiative using data from a rapid-cycle improvement program.